Hello, Welcome to the fifth part of chest Xray
Reading, today we shall know about the hilum and mediastinum
spare time to go through the other posts on
chest X ray
Here are the links
The Part 2 has over a lakh views, please go
through it.
Hilum
The normal hilar shadow is for 99% composed of vessels -
pulmonary arteries and to a lesser extent veins .
The vessel margins are smooth and the vessels have branches.
The left hilum should never be lower than the right hilum.
The left pulmonary artery runs over the left main bronchus,
while the right pulmonary artery runs in front of the right main bronchus,
which is usually lower in position than the left main bronchus.
Hence the left hilum is higher than the right.
Only in a minority of cases the right hilus is at the same
level as the left, but never higher.
In this illustration the lower lobe arteries are coloured
blue because they contain oxygen-poor blood.
They have a more vertical orientation, while the pulmonary
veins run more horizontally towards the left atrium, which is located below the
level of the main pulmonary arteries.
Both pulmonary arteries and veins can be identified on a
lateral view and should not be mistaken for lymphadenopathy
Sometimes the pulmonary veins can be very prominent.
The left main pulmonary artery passes over the left main
bronchus and is higher than the right pulmonary artery which passes in front of
the right main bronchus.
These images are thick slab sagittal reconstructions of a
chest-ct to get a better view of the hilar structures.
The lower lobe pulmonary arteries extend inferiorly from the
hilum.
They are described as little fingers, because each has the
size of a little finger .
On the right side the little finger will be visible in 94%
of normal CXRs and on the left side in 62% of normals.
IMPROVE YOUR X RAY READING SKILLS, BUY A BOOK. FIND ALL MEDICAL BOOKS ON FLIPKART WITH GREAT DISCOUNT
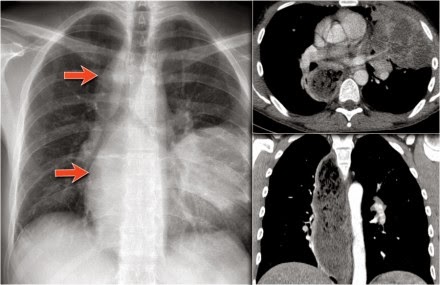
Study the CXR of a 70-year old male who fell from the stairs
and has severe pain on the right flank..
Notice on the PA-film the absence of the little finger on
the right and on the lateral view the increased density over the lower
vertebral column.
What is your diagnosis?
There is a right lower lobe atelectasis.
Notice the abnormal right border of the heart.
The right interlobar artery is not visible, because it is
not surrounded by aerated lung but by the collapsed lower lobe, which is adjacent
to the right atrium.
On a follow-up chest film the atelectasis has resolved.
We assume that the atelectasis was a result of
post-traumatic poor ventilation with mucus plugging.
Notice the reappearance of the right little finger (red
arrow) and the normal right heart border (blue arrow).
Hilar enlargement
The table summarizes the causes of hilar enlargement.
Normal hili are:
Normal in position
- left higher than right
Equal density
Normal branching
vessels
Enlargement of the hili is usually due to lymphadenopathy or
enlarged vessels.
In this case there is an enlarged hilar shadow on both
sides.
This could be the result of enlarged vessels or enlarged
lymph nodes.
A very helpful finding in this case is the mass on the right
of the trachea.
This is known as the 1-2-3 sign in sarcoidosis, i.e.
enlargement of left hilum, right hilum and paratracheal.
Here some more examples of sarcoidosis.
Lymphadenopathy
and groundglass appearance of the lungs
Lymphadenopathy,
1-2-3 sign
Bulky
lymphadenopathy
1-2-3 sign
Nodular lung
pattern, no lymphadenopathy
Hilar and
paratracheal lymphadenopathy
Mediastinum
Here is just a brief overview of Mediastinal
masses.
The mediastinum can be divided into an anterior, middle and
posterior compartment, each with it's own pathology.
Mediastinal lines
Mediastinal lines or stripes are interfaces between the soft
tissue of mediastinal structures and the lung.
Displacement of these lines is helpful in finding
mediastinal pathology, as we have discussed above.
Azygoesophageal recess
The most important mediastinal line to look for is the
azygoesophageal line, which borders the azygoesophageal recess.
This line is visible
on most frontal CXRs.
The causes of displacement of this line are summarized in
the table.
A hiatal hernia is the most common cause of displacement of
the azygoesophageal line.
Notice the air within the hernia on the lateral view.
HERE IS A SMALL BUT QUITE INFORMATIVE BOOK ON CHEST X RAY DOCTORS SHOULD READ, THERE IS GOOD COLLECTION OF BOOKS ON FLIPKART
Another common cause of displacement of the azygoesophageal
line is subcarinal lymphadenopathy.
Notice the displacement of the upper part of the
azygoesophageal line on the chest x-ray in the area below the carina.
This is the result of massive lymphadenopathy in the
subcarinal region (station 7).
There are also nodes on the right of the trachea displacing
the right paratracheal line.
On the PET we can appreciate the massive lymphadenopathy far
better than on the CXR.
There are also lymphomas in the neck.
this is an important finding, since these nodes are
accessible for biopsy.
Continue with images of CT and ultrasound.
Here we see a CT-image.
The azygoesophageal recess is displaced by lymph nodes that
compress the left atrium.
The final diagnosis of small cel lungcancer was made through
a biopsy of a lymphnode in the neck.
First study the chest x-ray.
Then continue reading.
Notice the following:
There is
displacement of the azygoesophageal line both superiorly an inferiorly.
There is an
air-fluid level (arrow).
Combined with the
above this must be a dilated esophagus with residual fluid. The final diagnosis
was achalasia.
The density on the
left in the region of the lingula is the result from prior aspiration
pneumonia.
Here we have a prior CXR of this patient.
The AP-film shows a right paratracheal mass.
The azygoesophageal recess is not identified, because it is
displaced and parallels the border of the right atrium.
The large round density in the left lung is the result of
aspiration.
Notice the massive dilatation of the esophagus on the CT.
Aortopulmonary window
The aortopulmonary window is the interface below the aorta
and above the pulmonary trunk and is concave or straight laterally.
Here the AP-window is convex laterally due to a mass that
fills the retrosternal space on the lateral view.
On the CT-images a mass in the anterior mediastinum is seen.
Final diagnosis: Hodgkins lymphoma.
Here another case.
On the PA-film a mass is seen that fills the aortopulmonary
window.
The PET better demonstrates the extent of the lymphnode
metastases in this patient.
Final diagnosis: small cell lungcarcinoma.