Breath sounds made easy.
To understand breath sounds ,we should first stress
on the Anatomy & Physiology of lungs.This is important
as we have to know where & how & why these sounds
are produced.Don't forget to check the Audio links at the
end of the post.
Lobes of Lung & their surface markings:
The right & left lung are divided by deep fissures into lobes.

Surface markings:
This is very important for us to localize the lesion in lung.


The right & left lung are divided by deep fissures into lobes.
| Right lung | Left lung |
|
|
|
|
|
|

Surface markings:
This is very important for us to localize the lesion in lung.


Areas of Auscultation:


Breath Sounds:
| Normal | Abnormal | Adventitious |
| Tracheal | Absent/decreased normal breath sounds | Crackles (rales) |
| Bronchial | Bronchial sounds in abnormal areas. | Wheeze |
| Bronchovesicular | Rhonchi | |
| Vesicular |
Normal Breath Sounds
To be able to distinguish between types of abnormal breath sounds and know their location,
it is important to understand normal respiration and its effect on airway noises that make up breath sounds.

- Normal respiratory cycle

- The inspiratory phase is shorter with faster airflow.
- The majority of breath sounds, both normal and adventitious, are in the range of 16 to 200 Hz.
- This is at the lower end of the spectrum of normal hearing (16 to 16,000 Hz).
- The sensitivity of the human ear in detecting low-frequency sound is relatively poor;
- thus, breath sounds are difficult to appreciate even with the stethoscope.
| Normal Breath Sounds | Normal Location of Sound | Sound Quality | Distinguishing Characteristic | Diagram |
| Tracheal | Only heard over the trachea. | loud, harsh like air is being blown through a pipe. | Expiration slightly longer than inspiration with similar loudness & a pause between. | 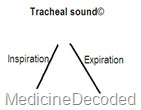 |
| Bronchial | present over the large airways & thus heard over the body of the sternum | these sounds are more tubular and high pitched than vesicular sounds, but not as harsh as tracheal breath sounds. | Expiratory sounds are louder & last longer than inspiratory sounds & have a short pause between inspiration and expiration sounds |  |
| Bronchovesicular | heard in the posterior chest between the scapulae and in the first & second intercostal spaces anteriorly. | medium pitched | Inspiration & expiration sounds equal in length& loudness.these sounds are different from vesicular since they have a pause between inspiration & expiration. | 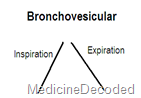 |
| Vesicular | heard throughout most of the lung fields( Periphery of lungs) | soft, low pitched, or rustling sounds normally | Inspiration sound is longer & louder than expiration sound without a pause between them. |  |
You can have a peek into the various sounds for better understanding by pressing the image below.

Important :Now you may get the doubt that "why the Vesicular sounds have increased
inspiratory time& loudness than expiration sounds which is contradictory to what we
have learnt in the beginning of the post about Respiratory cycle?"
The reason is in the below image-


Important :Now you may get the doubt that "why the Vesicular sounds have increased
inspiratory time& loudness than expiration sounds which is contradictory to what we
have learnt in the beginning of the post about Respiratory cycle?"
The reason is in the below image-

Abnormal Breath sounds:

The above so called Normal Breath sounds are considered normal only when they are heard in their
respective places ,if they are heard in a different place ,they are abnormal.
Bronchial sounds:
- When auscultated in other areas, bronchial breath sounds are an abnormal finding.
- They are heard over areas of consolidation, as solid lung conducts the sound of turbulence in
This very hollow or amphoric sound has been likened to that heard when air passes over the top
of a hollow jar (Greek amphoreus).
| Causes of bronchial breath sounds( ie, in areas other than over body of sternum) |
| Common |
| Lung consolidation (lobar pneumonia) |
| Uncommon |
| Localised pulmonary fibrosis |
| Pleural effusion (above the fluid) |
| Collapsed lung (eg: adjacent to a pleural effusion) |
ADVENTITIOUS SOUNDS:
- Added lung sounds are divided into two general groups: discontinuous sounds,
250 milliseconds .
Some clinicians maintain that the timing of onset of crackles aids in the differential diagnosis of parenchymal
- Discontinuous sounds are further classified as either coarse or fine crackles; continuous sounds,
- explosive, sharp, discrete bursts of interrupted sound.
- Their pattern is remarkably constant and cannot be destroyed by coughing.
- Crackles are divided into two types depending on their acoustic properties.
| Fine Crackles | Coarse Crackles |
| sounds like the crackling noise made when salt is heated on a frying pan. | sound of water being poured from a bottle. |
| On auscultation fine crackles are in general higher pitched, less intense and of shorter duration than coarse crackles. | coarse crackles are in general lower pitched, less intense and of longer duration than fine crackles. |
| The probable mechanism for the production of fine crackles is as follows. During inspiration, the air pressure on the "upstream" (mouth) side increases until it is able to overcome the forces that are closing the bronchiole. When this occurs, the airway snaps open as the pressure between the bronchiole and the alveolus is equalized . The resulting vibration in the airway causes a discrete, sharp sound of very short duration. | The bubbling sound of coarse crackles is produced when air passes over secretions in the larger airways (trachea and bronchi). |
| Fine crackles are usually appreciated only during inspiration. | Since air flows through the airways during inspiration and expiration, coarse crackles are more likely to be detected during both phases of the respiratory cycle. |
| The most common conditions associated withcoarse crackles are congestive heart failure and pneumonia,Bronchiectasis. | |
- Consistent with its mechanism ,crackles are typically predominant in lung bases ,where the
- As hundreds of airways open sequentially, the characteristic crackling sound is produced. The sound
Some clinicians maintain that the timing of onset of crackles aids in the differential diagnosis of parenchymal
and airways-disease.
- Crackles auscultated during early inspiration are thought to be more indicative of airways disease,
- Crackles auscultated during late inspiration are more suggestive of parenchymal disorders, such as
| Early inspiratory crackles | Mid to Late inspiratory crackles |
| Dependent atelectasis | Bronchiectasis |
| Bronchitis | Restrictive lung diseases
|
| Asthma | pulmonary edema |
| Emphysema |
Continuous:
- wheeze
- rhonchi

Wheezes are divided according to timing in respiratory cycle & actual sound produced ( monophonic or polyphonic)
Polyphonic wheeze:
- the most common type
- typical of COPD & asthma
- multiple simultaneous different pitched sounds occur during expiration & signify diffuse airway disease
- note of single pitch resulting from narrowing of a single airway
- sound does not change with coughing
- seen in tumor or foreign body case
- caused by vibration after opening of previously closed airway
- typical of extrinsic allergic alveolitis
- Stridor is a continuous, high-pitched monophonic sound heard throughout respiration; this sound is
- implies local obstruction to extra-thoracic airways (which tend to collapse on inspiration)
- often implies carcinoma or foreign body in major airways

Pleural rub:
- The visceral and parietal pleurae normally move silently against each other during respiration.
- However, when the pleurae are inflamed, the two thickened surfaces produce vibrations as they
- A pleural rub is the sound produced by the motion of inflamed pleurae. It tends to be a loud, grating
and expiration.
- A pleural rub has also been described as a leathery sound. Usually, the inspiratory and expiratory
- When effusion separates the two pleural surfaces, the rub may disappear. However, the disappearance
it can usually be distinguished from a pleural rub by having the patient hold his breath. During breath-holding,
a pleural rub disappears but a pericardial rub persists.
Mediastinal crunch (Hamman's sign)
- grating, crunching sound heard in the center of the anterior chest. The sound coincides with the heartbeat
clear, however, it may involve compression of the air by the beating heart and the mediastinal structures.
- heard over the precordium in spontaneous mediastinal emphysema.
- This sound is heard best over the left lateral position. It has been described as a series of precordial
pneumomediastinum or pneumopericardium, and is associated with tracheobronchial injury due to trauma,
medical procedures (e.g., bronchoscopy) or proximal pulmonary bleb rupture. It is commonly seen in
Transmitted voice sounds:
Egophony, bronchophony, and pectoriloquy all refer to auscultatory signs that can be heard over areas of
pulmonary consolidation. The pathogenesis of these signs relates to the increased sound transmission through
the consolidated lung. This results in transmission of sound-from the larger bronchi through the consolidated
lung to the periphery without significant loss in sound quality.
CLINICAL CORRELATIONS
generally correlates with the degree of obstruction. Breath sounds at the mouth will be heard at normal
intensity.
| Transmitted voice sounds | Location of sound | Method of elicitation | Reason( since sound travels faster & better in solids, liquids compared to in air) |
| Egophony | over consolidated lung tissue | elicited by having the patient say the letter "E' while you listen with the stethoscope. When egophony is present the "E" sounds like "A." | Mass/exudate in the lungs enables greater transmission of sound of patient repeating letter "E" |
| Bronchophony | over consolidated lung tissue | demonstrated by having the patient say a phrase as you auscultate; "ninety-nine" is the conventional phrase. The sound will be indistinct and muffled over the normal lung. However, the "ninety-nine" will be heard distinctly over the consolidated lung, without loss of clarity. | Mass/exudate in the lungs enables greater transmission of sound of patient repeating number "99" |
| Whispering Pectoriloquy | over consolidated lung tissue | similar to bronchophony, except it is usually elicited by having the patient say the phrase "one, two, three." The phrase will be muffled and indistinct when you auscultate over the normal lung and clearly audible when you auscultate over an area of consolidation. | Mass/exudate in the lungs enables greater transmission of sound of patient whispering |
CLINICAL CORRELATIONS
- The common obstructive diseases of the lung - chronic bronchitis, emphysema, and asthma -
- Patients with chronic bronchitis commonly have noisy chests because of crackles and wheezes.
generally correlates with the degree of obstruction. Breath sounds at the mouth will be heard at normal
intensity.
- Patients with emphysema, on the other hand, present with a relatively quiet chest. Breath sounds are
is present.
- The expiratory phase of vesicular breath sounds is similarly prolonged, however, breath sounds heard at the
- Polyphonic Wheezing is the hallmark of clinical asthma & COPD. In patients with mild or early asthma,
the wheezes are heard over the entire chest and in both phases of respiration. The breath sounds are
vesicular, and there is a prolonged expiratory phase that tends to correlate with the degree of bronchial
obstruction. Breath sounds heard at the mouth are of normal intensity. Interstitial pneumonitis and fibrosis
are characterized by the presence of fine inspiratory crackles. With early or mild disease, the crackles are
heard at end-inspiration; however, as the disease progresses, they may occupy more of the inspiratory
cycle - it is often difficult to hear the underlying breath sounds because of the intensity of the crackles
in interstitial fibrosis, but the sounds are vesicular with no prolongation of expiration.
- Pulmonary consolidation, as in lobar pneumonia, yields bronchial breath sounds over the affected area.
- Left-sided heart failure. Pulmonary congestion associated with left sided heart failure is characterized by
- Breath sounds in left-sided heart failure are vesicular, although they sometimes have a prolonged expiratory
edema, while coarse crackles and polyphonic wheezes occur in severe pulmonary edema.
- Pleural effusion. Pleural fluid or pleural thickening muffles the transmission of all lung sounds to the
bronchial breath sounds are sometimes heard at the area just above the pleural effusion. The reason for
this is,the compressed edematous lung, which is immediately above the effusion, acts as a consolidation
and causes increased sound transmission.
- Pneumothorax. With a small or mild pneumothorax, decreased vesicular breath sounds may be heard on




No comments:
Post a Comment
Please leave your comments